Quick Useful Links
Pedors® shoes provides a FREE resorce to finding foot care professionals in your area, it is a website called LetsWalk.com. Many of these foot wear professionals will fit shoes and bill Medicare under Medicare's Shoes For Diabetics Program.
Patient Information on the Medicare Benefit for Therapeutic Footwear for Diabetics
In May 1993, Congress amended Medicare statutes to provide partial reimbursement for depth shoes, custom molded shoes, and shoe inserts or modifications to qualifying Medicare Part B patients with diabetes.
Here is a quick printable guide [CLICK THE IMAGE & PRINT] and there is more detailed information below this quick guide.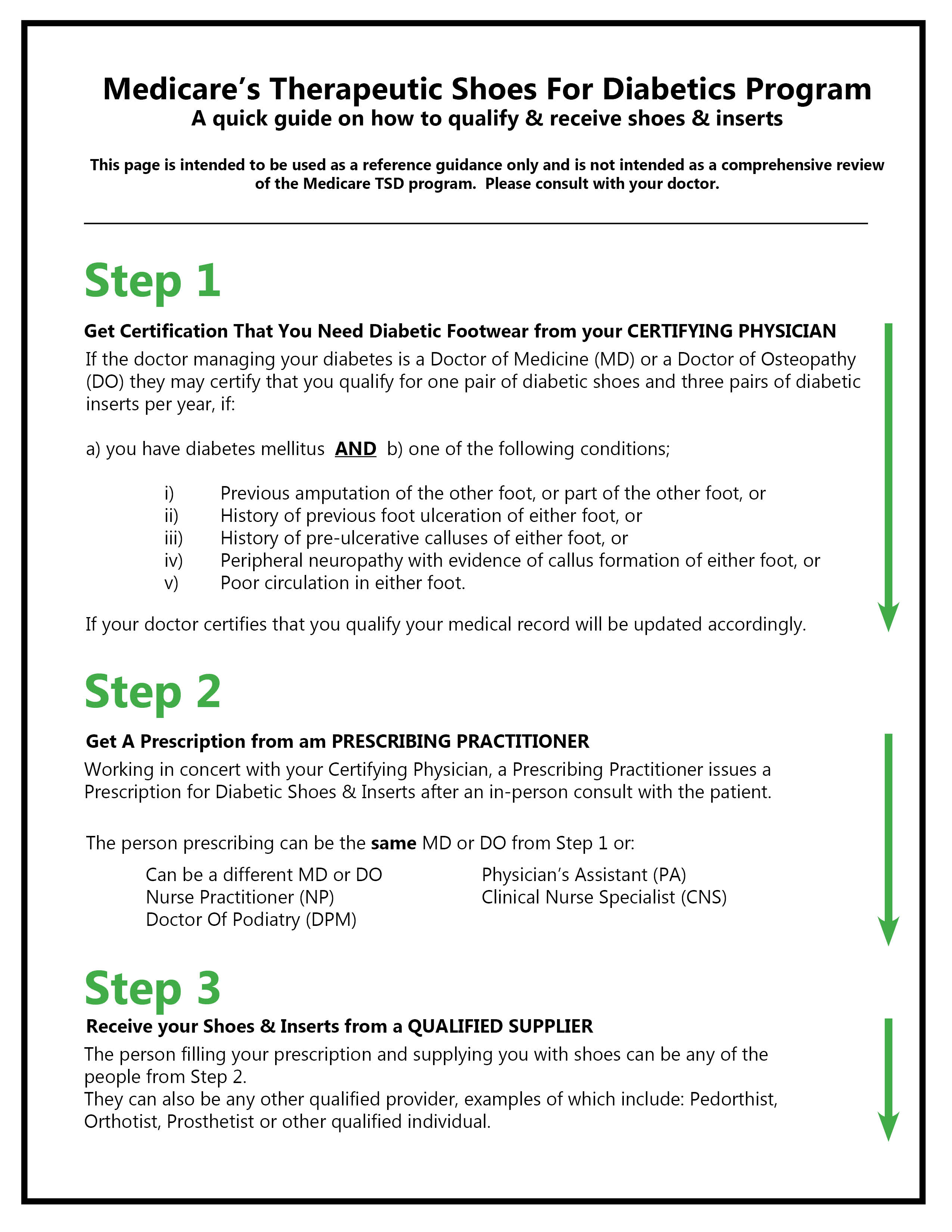
How Patients Qualify
The physician (M.D. or D.O.) who manages the patient's systemic diabetic condition is called the certifying physician. The certifying physician must state that the patient has diabetes mellitus, indicate what condition (s) is placing the patient at risk, and state that the patient is being treated under a comprehensive plan of care for his/her diabetes and needs therapeutic shoes and/or inserts because of the diabetes. The qualifying conditions are:
a. previous amputation of the other foot, or part of either foot, or
b. history of previous foot ulceration of either foot, or
c. history of pre-ulcerative calluses of either foot, or
d. peripheral neuropathy with evidence of callus formation of either foot, or
e. foot deformity of either foot, or
f. poor circulation in either foot;
The certifying physician may not supply the footwear unless he or she is the only qualified individual operating in the geographical area serving the beneficiary's address.
3 Step Process
Step 1
For a qualified patient to receive this benefit, the certifying physician (M.D. or D.O.) must conduct an in-person visit with the patient during which diabetes management is addressed within 6 months prior to delivery of the shoes/inserts, review and sign a "Statement of Certifying Physician for Therapeutic Shoes" prior to the dispensing of the devices.
Step 2
The next step is for the prescribing physician (D.P.M., M.D. or D.O.) to complete an appropriate prescription which will document the patients qualifying condition and the prescription for the appropriate diabetic footwear to address the condition and instructions for any modifications that may need to be made.
Step 3
With the prescription, the patient can then see a qualified provider who may be pedorthist, orthotist, prosthetist, or podiatrist to have the prescription filled following an in-person evaluation by the supplier. For traditional fee-for-service Medicare patients, the supplier will keep the documentation on file and submit the claim to Medicare on behalf of the patient. NOTE: Suppliers may not be able to dispense or submit claims for devices to Medicare patients enrolled in Medicare managed care plans.
A Podiatrist could be both the prescribing physician and a qualified provider. If the Podiatrist does not accept Medicare assignment the patient can take the prescription to a qualified pedorthist, orthotist or prosthetist who does. Dependent upon your State licensing laws, some pharmacists are also qualified providers. The prescribing physician should be able to direct the patient to a local qualified provider that accepts Medicare assignment.
Step 4 - Where To Go With Your Prescription
We think the best place to start is to see if there is a Pedorthist near where you live. To determine that go to the Pedorthic Footwear Associations web site and use their Pedorthist locator. If there is one near you, call to ask if they take Medicare assignment for diabetic shoes ( most do but some do not) and then make an appointment. The Pedorthist will evaluate and if he or she thinks the Pedors are the best option for you they can then order and bill Medicare for you. There is, as you probably know, a 20 % co-pay.
Medicare Reimbursement directly to the Patient
If the local prescribing physician does not accept Medicare assignment, and there is not a local qualified provider that does, the patient has the option of paying the provider the entire amount, and then applying for reimbursement directly from Medicare for 80% of the allowable amount. The Centers for Medicare & Medicaid Services (CMS) will reimburse 80% of the amount it designates as "allowable,” and the patient is responsible for paying 20% of the total payment amount. In order to qualify for coverage the patient must be fitted by a qualified provider, so it is not possible for a patient to purchase footwear directly from a manufacturer or a retail facility or online e-commerce store and then request the 80% reimbursement from Medicare.
NOTE: Some Medicare suppliers may not accept assignment if the allowable amount is too low to cover the appropriate materials and services. In these situations, the total cost to the patient may be higher than the allowable amount. If so, the patient may be expected to pay the Medicare supplier in full before he or she receives reimbursement from Medicare.
What is Reimbursable
Within a given calendar year, the qualifying patient can receive 80% of the allowed amounts for one pair of depth shoes and three pairs of inserts (not including the non-customized removable inserts provided with such shoes);
OR one pair of custom molded shoes (which include 1 pair of inserts) and two additional pairs of inserts.
Also: 1) shoe modifications can be substituted for an insert; and 2) custom molded shoes are only covered when the patient has a foot deformity that cannot be accommodated by a depth shoe.
The inserts can be either direct-formed prefabricated inserts that have been heat molded OR custom-molded inserts that have been individually fabricated for you.

